Abstract
Previous studies and meta-analyses addressing COVID-19 in patients with hematological malignancies (HM) have reported dramatically high mortality rates of up to 34% [Vigenthira 2020, Garcia-Suarez 2020, Sharafeldin 2021]. These studies, however, were strongly biased towards hospitalized patients, and poorly represented patients who experienced a milder course of COVID-19, not requiring hospitalization. Jerusalem and its metropolitan area, comprising of over 1.3 million inhabitants, was the epicenter of Israel's COVID-19 crisis, with over 200,000 cases. Hadassah Medical Center, one of only two tertiary centers serving this multi-ethnic population, houses a Hematology Department that includes inpatient services, a hematopoietic stem cell transplant (HSCT) center, day care services and in-campus outpatient clinics. From February 20 th, 2020, we tracked patients with confirmed COVID-19 reporting to their treating hematologists while being hospitalized due to COVID-19, at routine visits to the hematology services, or remotely via phone or email communication. This assured the representation of COVID-19 cases of various clinical severities. Data were collected retrospectively and included demographics, comorbidities, hematological diagnoses and treatments, course of COVID-19 and, importantly, source of infection. Univariate and multivariate analyses were used to assess association between prognostic factors and outcomes including hospitalization, severe COVID-19 (per updated WHO criteria) and critical COVID-19, defined as a composite of ICU admission and mortality. Almost all the patients in this series were diagnosed prior to their vaccination. To the best of our knowledge, this is the largest single center series of HM patients with COVID-19 reported to date.
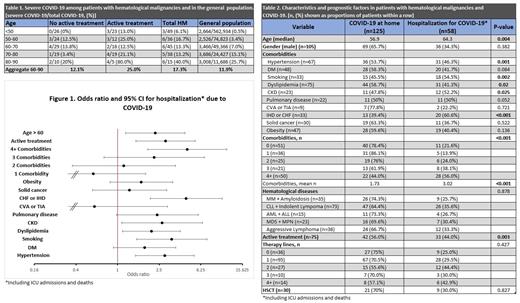
Our series included 183 patients. Median age was 62.5 years, 57% were men, and 72% had at least one comorbidity. The most frequent hematological diagnoses were indolent lymphoma and CLL (40%), aggressive lymphoma (20%) and multiple myeloma (19%). At the time of COVID-19 diagnosis, 41% of the patients were receiving systemic anti-neoplastic treatment (excluding TKIs for CML and hydroxyurea for MPN), and 16% had undergone a previous allogeneic or autologous HSCT. Overall mortality, severe COVID-19, and hospitalization rates in the entire group were 9.8%, 14.2% and 32%, respectively, remarkably lower than in previous reports. Of the patients not receiving anti-neoplastic treatment, mortality and severe COVID-19 rates were comparable to those of the age-matched general population according to the Israeli Ministry of Health database [Table 1]. Consistent with previous studies, ischemic heart disease (IHD), dyslipidemia, chronic kidney disease, smoking and hypertension, as well as age and active anti-neoplastic treatment, each emerged as a risk factor significantly associated with hospitalization due to COVID-19 [Fig. 1, Table 2]. IHD, smoking, age and active treatment remained significant in multivariate analysis. Age and active treatment as well as ≥4 comorbidities were significantly associated with critical COVID-19. Interestingly, we observed a strong association between the number of prior anti-neoplastic treatment lines and critical COVID-19. Neither history of HSCT nor treatment with monoclonal antibodies were associated with COVID-19 outcomes. Notably, we did not detect any patient that contracted COVID-19 within the Hematology Department services, both inpatient and outpatient.
Taken together, we present a different COVID-19 severity landscape in patients with HM as compared to previous observations. While active treatment was significantly associated with COVID-19 hospitalization and mortality, these rates were remarkably lower than previously reported. Despite harboring various degrees of immune suppression, patients with stable or indolent diseases not receiving active treatment appeared to be at a risk comparable to that of the age-matched general population, which depended largely on age and comorbidities. Routine preventive measures including symptom questioning, masks, and social distancing in both our inpatient and outpatient services provided a COVID-19-safe environment, obviating the need for changes in treatment schedules or assignment. These findings may have important consequences for future management of patients with HM in COVID-19 affected regions.
Lavie: AbbVie: Membership on an entity's Board of Directors or advisory committees, Other: Fees for lectures; BMS: Membership on an entity's Board of Directors or advisory committees; Takeda: Other: Fees for lectures; Roche: Other: Fees for lectures; Novartis: Other: Fees for lectures; Takeda: Consultancy. Goldschmidt: AbbVie: Consultancy, Research Funding.